Achilles tendons must have been rupturing since the time of Achilles. How else would every 40- 60-year-old male weekend warrior (and a number of pro basketball players) have learned to recognize and dread that classic gunshot sound of the tendon snapping?
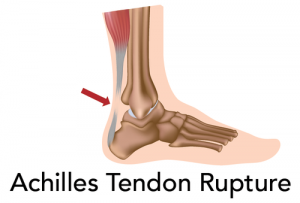
The Achilles tendon connects the muscles of the calf to the calcaneus, or heel bone. It is designed to stretch. This serves to absorb force as an athlete lands from a jump, and to deliver power to the foot in walking and running [1]. The tendon tissue is flat, with a good blood supply, and serves most women well for their entire lifetime [2]. Why does it vex men in the fourth and fifth decades, and why is the repair so troublesome?
The answer, like most in medicine, is multifactorial--an awful word that means "many contributing causes." Men traditionally play ballistic sports, at levels beyond what their fitness might warrant, well into their later years. A testosterone- driven competitive edge pushes them to leap higher, land harder and lunge further, going for that shot that is just out of reach. Their risk factors seem clear.
But what about women athletes? It's not fully understood. Though women are often also super fit, they are less likely than men to rupture their Achilles. According to one study, the Achilles tendons of women may be more elastic than those of men, which may contribute to their reduced incidence of tearing [3].
Treatments for those who are most at risk, however, continue to improve [4]. Surgical repair for complete ruptures is almost always recommended in the US, though non-operative healing is more common in other countries [5]. The outcomes appear to favor surgical repair if a return to sports with full athletic power is desired.
Techniques of surgical repair vary widely [6]. At the Stone Clinic we almost always perform a percutaneous repair, avoiding the classic long open incisions. Our rationale is that by pulling the ends of the tear together with a novel suture technique--which preserves the natural blood clot around the torn tissues--healing will be faster and better, with less risk of scarring or infection. We've shown excellent results with this technique for 20 years. Other surgeons prefer an open incision approach. Again, the results are usually excellent. The risk of infection, re-rupture and scarring, however, is higher with open surgical techniques [7].
Many patients are frustrated with the long rehabilitation process, no matter which technique is used. The post-operative program has become more aggressive over time, with earlier range-of-motion and weight-bearing exercises than ever before [8]. Manual physical therapy with daily soft tissue massage decreases scarring [9]. The healing process is augmented by injections of growth factors and/or stem cells, both at the time of surgery and during the recovery program [10].
While novel new growth factor and stem cell treatments may speed tendon healing, return to full sports still takes six months; the tissue has to both heal and strengthen to avoid re-rupture. The questions we ask in the 21st century are: Can these injuries be prevented? Could new scanning techniques identify Achilles tendons at risk? Could certain supplements speed the strengthening of the tendon after repair? And can we make the phrase "his Achilles heel" obsolete?
References
1. Novacheck, T. F. (1998). The biomechanics of running. Gait & posture, 7(1), 77-95.
2. Ahmed, I. M., Lagopoulos, M., McConnell, P., Soames, R. W., & Sefton, G. K. (1998). Blood supply of the Achilles tendon. Journal of orthopaedic research, 16(5), 591-596.
3. Achilles Tendon Biomechanics in Response to Acute Intense Exercise
Joseph, Michael F.1,2,3; Lillie, Kurtis R.1,2; Bergeron, Daniel J.1,2; Cota, Kevin C.1,2; Yoon, Joseph S.1,2; Kraemer, William J.1,3; Denegar, Craig R.1,2,3
4. Ronel, D. N., Newman, M. I., Gayle, L. B., & Hoffman, L. A. (2004). Recent advances in the reconstruction of complex Achilles tendon defects. Microsurgery, 24(1), 18-23.
5. Soroceanu, A., Sidhwa, F., Aarabi, S., Kaufman, A., & Glazebrook, M. (2012). Surgical versus nonsurgical treatment of acute Achilles tendon rupture. The Journal of Bone & Joint Surgery, 94(23), 2136-2143.
6. Wong, J., Barrass, V., & Maffulli, N. (2002). Quantitative review of operative and nonoperative management of Achilles tendon ruptures. The American Journal of Sports Medicine, 30(4), 565-575.
7. Khan, R. J., Fick, D., Keogh, A., Crawford, J., Brammar, T., & Parker, M. (2005). Treatment of acute Achilles tendon ruptures. The Journal of Bone & Joint Surgery, 87(10), 2202-2210.
8. Huang, J., Wang, C., Ma, X., Wang, X., Zhang, C., & Chen, L. (2014). Rehabilitation Regimen After Surgical Treatment of Acute Achilles Tendon Ruptures A Systematic Review With Meta-analysis. The American journal of sports medicine, 0363546514531014.
9. Shin, T. M., & Bordeaux, J. S. (2012). The role of massage in scar management: a literature review. Dermatologic Surgery, 38(3), 414-423.
10. Young, R. G., Butler, D. L., Weber, W., Caplan, A. I., Gordon, S. L., & Fink, D. J. (1998). Use of mesenchymal stem cells in a collagen matrix for Achilles tendon repair. Journal of Orthopaedic Research, 16(4), 406-413.