For many of us, our cell phone is our lifeline. It is how we connect with others via calls, text messages and emails, through pictures, social media and maybe even games with friends.
For some of us, cell phones are literally lifelines -- devices that monitor our health and transmit data to medical professionals, either routinely on an emergency basis.
It's fascinating, really, what can be done. With the right attachment and/or app, your phone can already track your heart rate, blood pressure, blood sugar and more. Between what exists and what's coming, the virtual checkup may be closer than you think.
In the rapidly changing world of healthcare technology, Dr. Eric Topol of The Scripps Research Institute is one of the preeminent thought leaders and visionaries. It is my privilege to turn this space over to him -- and one of his patients, Kim Goodsell -- to continue the conversation about these lifesaving innovations.
---
 Perhaps the best way to get a glimpse of the future of medicine is through the lens of a patient. One of us (Kim Goodsell) developed two extremely rare and very different, complex medical conditions involving the heart (arrhythmogenic right ventricular cardiomyopathy) and the nervous system (Charcot-Marie-Tooth). Ultimately, the root cause for both of these seemingly unrelated conditions turned out to be a mutation in a single gene, and the patient made the diagnosis herself through extensive Web-based literature and database searching that culminated in DNA sequencing. Because of the heart rhythm disorder, her physician (Eric Topol) advised her to have a smartphone electrocardiogram (ECG) app that enabled capturing of the heart rhythm at any time there was a cause for concern. Using the app for other purposes was not anticipated.
Perhaps the best way to get a glimpse of the future of medicine is through the lens of a patient. One of us (Kim Goodsell) developed two extremely rare and very different, complex medical conditions involving the heart (arrhythmogenic right ventricular cardiomyopathy) and the nervous system (Charcot-Marie-Tooth). Ultimately, the root cause for both of these seemingly unrelated conditions turned out to be a mutation in a single gene, and the patient made the diagnosis herself through extensive Web-based literature and database searching that culminated in DNA sequencing. Because of the heart rhythm disorder, her physician (Eric Topol) advised her to have a smartphone electrocardiogram (ECG) app that enabled capturing of the heart rhythm at any time there was a cause for concern. Using the app for other purposes was not anticipated.
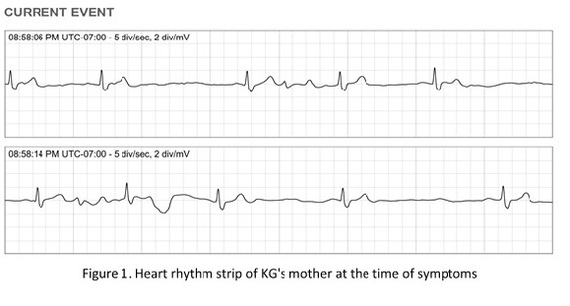
But recently KG's 81-year-old mother, Patricia Pfeffer, who had no prior heart problems, had an episode of marked dizziness and shortness of breath. Using the smartphone ECG, Patricia's heart rhythm was recorded (see figure below) and another mobile app showed her blood pressure to be 187/96. A computer algorithm interpretation diagnosed this was "serious" with a "wide QRS complex" very slow heart rhythm (rate 36) that required IMMEDIATE physician evaluation. Her daughter emailed the ECG strip to her physician (ET) and a referral for a pacemaker evaluation was made. With confirmation of complete heart block on further heart rhythm assessment, that was accomplished the following morning.
This case illustrates the ability for a patient to make the diagnosis of another patient at the point of need. With mobile apps and computer algorithms to interpret the data, the diagnosis could be made without the need for any physician. Rather than calling an ambulance or going to an emergency room to wait for an ECG to be performed, it was quickly done at the patient's home. It represents just the beginning of where unplugged medicine can take us.
Until now, the practice of medicine has largely been a one-off experience exemplified by single blood pressure measurements or annual physicals. A doctor drove the process, ordering snapshot blood tests or ECGs or scans. These were all done in hospitals, clinics, or central laboratory facilities. But with the era of unplugged medicine with smartphones, pervasive connectivity, and ubiquitous computing capability, all of this is about to change.
Beyond doing an ECG or blood pressure measurement, it is already technically possible to do most routine lab tests on a smartphone. These require a small hardware attachment or "add" just like the sensor case used to get the ECG. Algorithms can then rapidly interpret the data without the need for medical professionals. Of course, the accuracy and validation of all such technology has to be assured before it is made available to the public. That has already been done for the ECG app, approved by the FDA a couple of years ago. Many more are currently in the queue to be reviewed.
For the first time, we are able to get "real world" medical information about a patient instantaneously and inexpensively. Further, an individual can collect the data frequently or even continuously when necessary, instead of just on rare occasions. It is not hard to envision where this is headed. More sophisticated analytics, that integrate and process all the relevant data collected by an individual will likely be able to predict an illness before it ever happens, such as detecting an abnormality in lung function prior to even a wheeze, no less an asthma attack. Less need for hospitals to monitor patients is imminent since this can be readily done with the convenience, safety, and markedly reduced cost staying at home. These new capabilities of mobile medicine not only empower consumers, but also will undoubtedly reshape the future of how health care is rendered. We're thankfully moving away from pain points -- that everyone is all too familiar with -- to a new model of having critical data and information when and where it's needed.
Eric Topol is a cardiologist at Scripps Clinic, Chief Academic Officer at Scripps Health, Professor of Genomics and The Scripps Research Institute, and author of "The Creative Destruction of Medicine"
Kim Goodsell is a "Digital Patient Revolution" activist, co-Founder ProAbility WalKArt L3c, inventor of ROVA (Realtime Operational/ Virtual Assistant)