The knee is tied together by more than just the anterior cruciate ligament (ACL), though you might not know that hearing the daily reports of ACL injuries from football, soccer, basketball and skiing. The "other" ligaments matter just as much, and though injured less frequently, their care and feeding determine the function of the knee.
Let's go around the knee.
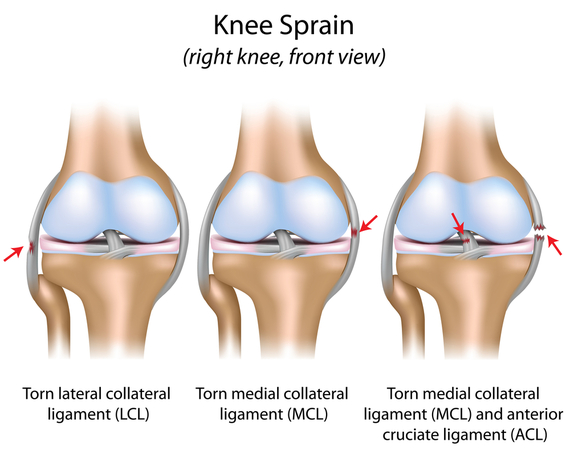
The medial collateral ligament (MCL) is the side ligament on the inside of the leg. It is often injured when a player is hit from the outside on the planted leg and the knee bends inward or when a ski catches an edge and shoots out to the side. Fortunately, the MCL, since it is on the outside of the joint with an excellent blood supply, almost always heals without surgery, as long as it is protected during the healing time and mild, but not deforming stress is applied. [8] This is achieved by moving the knee from 30-90 degrees and avoiding full extension and side stress.
The posterior cruciate ligament (PCL) crisscrosses the ACL, stopping the tibia from going backwards on the femur. It is most often injured in car accidents when the knee hits the dashboard and is driven backwards tearing the ligament. It rarely, if ever, heals successfully on its own. [2,4] Because the repair and reconstruction techniques for the PCL were difficult, many physicians still recommend non-operative care for PCL injuries. However, left untreated, knees with PCL ruptures often develop meniscus tears and arthritis. [6,9,12] The surgical techniques have improved so much that we usually repair or reconstruct this ligament with donor tissue of bone-patellar tendon-bone, the strongest substitute currently available.
The posterolateral corner of the knee (PLC) is not truly a ligament but a merger of soft tissues at the back (posterior), outside (lateral) corner of the knee. The area is significantly injured in up to 30 percent of ACL injuries, yet the injury is often missed, even when an MRI has been obtained. [10] It is diagnosed by a careful exam of the knee that demonstrates a dialing of the tibia off the femur when the leg is bent. Missing the diagnosis and failing to repair this corner when the ACL is reconstructed is a common cause of recurrent knee instability and ACL failure. [1,5,13] We rebuild this corner with a donor ligament, which almost always makes the knee feel more stable and protects the central ligaments.
The lateral collateral ligament (LCL) is injured much less frequently in sports, though an injury can occur if somebody were to cartwheel down a ski slope or get taken out with a side hit in football or soccer. The LCL can heal on its own, if the injury is isolated to the LCL, but when found in combination with ACL or PCL, the injury often needs to be repaired. The repair is usually done with sutures. [7]
The anterolateral ligament (ALL) is a thickening of the synovium (a layer of tissue which lines the joints and tendon sheaths) at the front outside of the knee. [3] It may be injured when the ACL is torn, and can be diagnosed with an MRI. Reinforcing this area with sutures, or on occasion with a graft, can provide additional stability to the ACL reconstruction, though we suspect it most often heals on its own.
So now you know, there are a lot of structures guiding the knee, all of which must be evaluated in any complex knee injury. When you hear about the athlete who injured his ACL, you might ask what else was injured. That answer will determine how well and how soon they return to sports.
Sources
1. Blackman AJ, Bogunovic L, Cherney S, Wright RW: Chapter 5 - Technical Causes of ACL Graft Failure. Revision ACL Reconstruction: Indications and Technique. Ed. Marx RG. Springer, pgs 43-52, 2013.
2. C.R. Allen, L.D. Kaplan, D.J. Fluhme, C.D. Harner
Posterior cruciate ligament injuries
Curr Opin Rheumatol, 14 (2) (2002), pp. 142-149
3. Claes S., Vereecke E., Maes M., Victor J., Verdonk P., Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013;223:321-328.
4. Harner CD, Hoher J. Evaluation and treatment of posterior cruciate ligament injuries. Am J Sports Med. 1998;26(3):471-482.
5. LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force. A biomechanical analysis. Am J Sports Med. 1999;27(4):469-475.
6. Logan M., Williams A., Lavelle J., Gedroyc W., Freeman M. The effect of posterior cruciate ligament deficiency on knee kinematics. The American Journal of Sports Medicine. 2004;32(8):1915-1922. doi: 10.1177/0363546504265005
7. Marks PH, Harner CD: The anterior cruciate ligament in the multiple ligament-injured knee. Clin Sports Med 12:825 -838,1993
8. P. Kannus. Long-term results of conservatively treated medial collateral ligament injuries of the knee joint.
Clin Orthop Relat Res. 1988 January; (226): 103-112.
PMID: 3335084
9. P.M. Keller, K.D. Shelbourne, J.R. McCarroll, A.C. Rettig
Nonoperatively treated isolated posterior cruciate ligament injuries
Am J Sports Med, 21 (1) (1993), pp. 132-136
10. Pacheco RJ, Ayre CA, Bollen SR. Posterolateral corner injuries of the knee: a serious injury commonly missed. J Bone Joint Surg Br. 2011;93(2):194-197.
11. Strobel M. J., Weiler A., Schulz M. S., Russe K., Eichhorn H. J. Arthroscopic evaluation of articular cartilage lesions in posterior cruciate ligament--deficient knees. Arthroscopy--Journal of Arthroscopic and Related Surgery. 2003;19(3):262-268. doi: 10.1053/jars.2003.50037.
12. W.B. Geissler, T.L. Whipple
Intraarticular abnormalities in association with posterior cruciate ligament injuries
Am J Sports Med, 21 (6) (1993), pp. 846-849
13. Wolf RS, Lemak LJ. Revision anterior cruciate ligament reconstruction surgery. J South Orthop Assoc. 2002;11(1):25-32.