When most healthy women consider their risk of getting breast cancer, they rarely view it as an immediate threat. Melanie Testa used to be one of those women -- until she was diagnosed with stage 3 breast cancer in January 2011. "I was frightened, I was afraid," she recalls. "I sort of went on emotional shutdown soon after. ... But you know, just like anything else in life, you pick up the pieces, you figure out what you need to do, and you move on to your next step."
For a growing number of women, that next step involves bilateral mastectomy (or removing both breasts -- even though cancer almost always affects just one). "[The number of] bilateral mastectomies have been going up in every report that I've seen," says Neil Fine, M.D., a plastic surgeon in private practice with Northwestern Specialists in Plastic Surgery in Chicago.
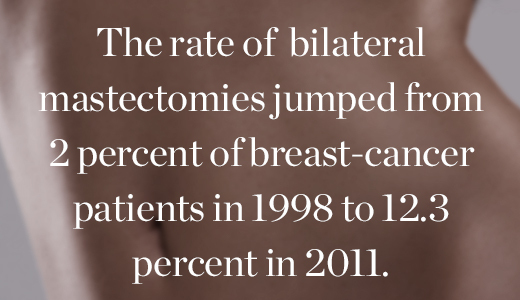
One 2014 study published in the Journal of the American Medical Association found that, among nearly 190,000 breast cancer patients studied, the rate of bilateral mastectomies jumped from 2 percent of patients in 1998 to 12.3 percent in 2011. (Among participants under 40, the spike was even more pronounced: The rate increased from 3.6 percent in 1998 to 33 percent in 2011.) And those numbers don't even include all of the women who, like Angelina Jolie, have opted to get bilateral mastectomies after learning they have BRCA1 or BRCA2 genetic mutations, which increase their odds of being diagnosed with breast cancer by the age of 70 four- or five-fold.
"If you have a known gene marker, then it really does seem that you are at a high risk for developing breast cancer," says Fine. "You have two possibilities: One is close surveillance, and the other is surgery. And I try to make sure [my patients] understand that -- that they have those choices."
Women who decide to undergo a bilateral mastectomy and to reconstruct afterward can choose implants or to use excess abdominal tissue or back tissue in lieu of implants. "The dominant one by far is implants," says Fine.
The difficult details that follow -- the decision of whether to opt for a nipple-sparing surgery or one that removes them, the two to four hours in surgery, the night in the hospital, the week or two spent dealing with drains in your chest following the surgery, the pain, the recovery, and the potential follow-up surgeries, depending on the exact procedure a woman chooses -- only tell part of the story of what getting a bilateral mastectomy involves.
"Hearing what other women go through can be a valuable, sort of eye-opening experience about what's out there," says Fine. "But it's not to be fooled that it will actually let them know what they're going to go through. They're going to go through a unique experience, and there's just no way around that. There's no way for every woman not to have her own unique experience."
With that caveat in mind, we interviewed and photographed four women who've undergone bilateral mastectomies; here's what they say their unique experiences entailed.
Melanie Testa, 46, was diagnosed with stage 3 breast cancer in January 2011 and underwent chemotherapy to reduce the size of her tumor prior to her mastectomy. Before surgery, she was a double D -- but she opted not to reconstruct, saying she was always uncomfortable with the idea of it.
"I was asked to see a psychiatrist after telling my breast surgeon that I did not want reconstruction and that I wanted my non-affected breast removed, as well. That hospital did not ask people who were getting reconstructive surgery with construction on the opposing breast to do the same. ... I am really happy to say that my surgeon listened to my wants and needs, trusted that I knew what I wanted, and did what I asked him to do. Not all women in my support groups had that, and as far as I'm concerned, that's not okay. Doctors need to start trusting that their patients know what they want.
"I think that, generally, 80 percent of my husband is perfectly fine with my decision. I don't think that he is in agreement with reconstruction. I know that he does not want to see reconstructed breasts on my body, but there is, of course, mourning. We both mourn the loss of my breasts, and there has been a period of time where he was in deep mourning for my breasts, and we are just about coming out on the other side of that. We're learning to talk about being flat-chested, about how it makes him feel. I think it's harder for men because they're not conditioned to evaluate emotions, so we're coming around. ...
"I love my body more than I ever have before. I feel like I look svelte, and I love the clothing that I am able to wear and I would have never worn prior to surgery. I love low, plunging necklines. It's like night and day. I just feel more comfortable in my body. I would love to have my breasts back, but I don't long for them. I like this body more."
Carol (not her real name), 30, was seeing a new doctor for the first time, running through her family's health history, when he suggested she undergo genetic testing. Two months later, she was sitting in a waiting room alone, waiting for her mother to wake up from a hysterectomy, when she got a phone call; Carol had the BRCA1 genetic mutation. After meeting with a genetic counselor, a breast surgeon, and a plastic surgeon, she decided to undergo a nipple-sparing bilateral mastectomy with reconstruction to drastically reduce her breast cancer risk. She had her surgery in December 2013. Today, she's five months pregnant. She won't be able to breastfeed because she's had too much breast tissue removed, but since some remains, she will produce enough milk to need nursing pads.
"The only thing that I'm not thrilled with -- but it's not the end of the world -- is just the lack of feeling afterward. It's something almost all women who have this surgery experience. When they take out the tissue, you lose the feeling in your breasts. ... In the beginning, I couldn't feel anything, but now I can feel more. They say give it five years, and then after five years, whatever you can feel, that's all you're going to feel. ... So it's the only thing that I'm not really a fan of, but I take that over possibly getting cancer any day."
"I definitely always wanted to breastfeed, and then I found this out and decided that it wasn't that important to me. It was important to me and I always wanted to do it and thought I would -- but reducing my risk of breast cancer was definitely more important to me. ... I'd rather have had this surgery and be healthy for my future children than to have breastfed and possibly develop breast cancer down the line."
Liz Gordon, 25, found the first lump in her breast when she was about 15. She had the fibroadenoma (a non-cancerous tumor) removed but found another one not too long afterward. Her doctor suggested she undergo genetic testing to see if she had the same BRCA2 mutation that her mother, who was struggling with breast cancer, did. At the age of 16, she learned that she did, in fact, have the mutation -- and so would likely get breast cancer at some point, given her family history. She decided to have a three-part double mastectomy with nipple reconstruction last year at the age of 24, about 10 years before the age at which her mother (who passed away in 2008) had been diagnosed. During the first surgery, her breasts were removed and expanders were put in. During the second surgery, the expanders were replaced with implants. During the third surgery, Liz's nipples and areola were reconstructed using skin from her inner groin.
"When I first had [my surgery] done, I wouldn't remove the bandages myself. I had my friend come over to do it with me. ... You kind of prepare as best you can, but you can't prepare for that. I knew I would see nothing [no nipples or areola], but I think what freaked me out more or in a different sense were the wounds and whatnot. It was crazy, and I'm sure it was crazy for [my friend] to see. ... But not having my mom there [because she'd passed away], my friend was the second person I could kind of fall back on. It was the best option I had."
"It's only recently that I'm just getting comfortable really sleeping. Not necessarily through the night, but finding a comfortable spot to sleep because I can't necessarily lay on my stomach; it puts too much pressure [on my breasts]. I still don't lift anything heavy because it just feels like too much. And depending on what I'm wearing or the weather, the groin area [where surgeons took skin to make Liz's nipple and areola] still irritates, but only in a couple of spots I would say, maybe just depending on where it healed differently."
Erika Stallings, 30, remembers when her mom was diagnosed with breast cancer in 1993 (they've known that she has the BRCA2 genetic mutation since 2007). Erika decided to get tested herself in 2014, when she was around the same age her mother had been at her diagnosis. When she received the results -- that she, too, had the gene mutation -- she consulted her genetic counselor and decided to undergo a nipple-sparing bilateral mastectomy in December 2014.
"I went in October to pick out the implants, and a guy friend came with me because I wanted a guy's opinion on what they felt like. It made me feel better because it was like, 'This is what I like,' but I wanted to know what he would like, too."
"The first time I woke up, I was like, 'Why did I do this? I can't believe that I did this. Why did I make this decision?' As time has gone on, they feel more like my breasts. If you had a comparison photo, they really do look almost entirely the same, so I've calmed down about it. The scar also seemed really massive at the beginning, and now you can't really tell. ...
"I'm happy to have done my surgery because it's just nice to not have to worry about it. It's not like this shadow hanging over my life. ... Everything after this kind of feels like a cakewalk. It kind of just makes you a little bit fearless."
---
If you're considering getting a mastectomy and want information or support -- or you're looking for more general information about how you can assess and/or lower your risk of breast cancer -- visit brightpink.org.
By Robin Hilmantel