Last year I saw a remarkable documentary, The Space Between, which chronicles the struggle of providing palliative care services in a Kenyan hospice setting through the stories of four individuals receiving care at Kimbilio Hospice (Kiswahili for Refuge). Kimbilio Hospice is a 24-bed, in-patient hospice that provides quality palliative care services to adults and children living with life-threatening illnesses. The hospice is managed by Living Room Ministries International (heretofore Living Room) which was established in 2009 and to this day, the care given at the hospice remains free of charge. Over the course year Juli McGowan Boit the founder of the hospice and filmmakers Kimberly Nunez-North & Travis North kindly shared with me their experiences.
Providing palliative care in emerging market health systems has unique challenges. One of the most pervasive is the understanding of palliative care and hospices as services provided prior to (an inevitable rapid) death. But as defined by the WHO, "Palliative care is an approach that improves the quality of life of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual." However the stigma related to death and dying run very deep in some communities and cultures. Another reality of low resource environments is how to allocate scarce resources. In Africa most of the financial resources and health infrastructure is directed at addressing communicable diseases such as HIV/AiDs, TB and malaria as well as child and maternal health.
Understanding how large the palliative care market is in Kenya is not a straight forward calculation. Juli McGowan Boit, is a nurse practitioner and HIV volunteer in rural Kenya who partnered with local leaders to found the Kimbilio Hospice, shared the following information. It is estimated that 1.6 million people are living with HIV/AIDS and according to Kenya's ministry of health, "cancer ranks third as a cause of death after infectious diseases and cardiovascular diseases. It causes 7% of total national mortality every year. Although population based data does not exist in the country, it is estimated that the annual incidence of cancer is about 28,000 cases and the annual mortality to be over 22,000. Over 60% of those affected are below the age of 70 years. In Kenya, the risk of getting cancer before the age of 75 years is 14% while the risk of dying of cancer is estimated at 12%." According to the WHO, "at least 50% of HIV patients and 80% of cancer patients will suffer from severe pain in the course of the terminal phase of their disease." As Juli made clear, "all of these patients would benefit from palliative care, if it was available and affordable."
What Juli McGowan Boit, and the filmmakers Kimberly Nunez-North & Travis North are doing is changing the narrative of palliative care, how it can be administered and its impact in some of the most trying conditions.
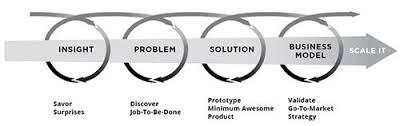
The consistency of Living Room's approach to caregiving on both a patient and community level has yield, intentionally or not, a model example of the "The Innovator's Method" - insight, problem, solution, business model, scale it. An example of this is their Kimbilio Funeral Home. The funeral home serves the hospice as well as the larger community.
(source the Innovator's Method)
- Insight: Living Room met with members of the community for over a year before starting the business in 2012 to make sure that it was a service they wanted within the village.
- Problem: The nearest mortuary is located in a town about an hour's drive away from the hospice
- Solution: A funeral home within the community provides manageable accessibility (reduced travel) as well as reducing costs for the families. The services include embalming and storage, casket sales, flowers and programs. The funeral home also offers a vehicle for hire that serves as a hearse as well as tents and chairs that can be rented for funeral services.
- Business model: The funeral home has been open for three years and is currently covering 15% of Kimbilio Hospice operating expense.
- Scaling it: Living Room anticipates the funeral services will cover up to 25% of the hospice's operating expenses within the next year.
Since the release of The Space Between there have been some notable developments and welcomed surprises. First is that the documentary was embraced by an unanticipated audience, nursing schools and the medical education community. Kimberly explained, "We didn't set out to make a film that could be used as an educational tool. I was actually shocked given that the medical advancements in the USA are much greater than the resources available in Kenya. However, after talking to many hospice providers and educators, it became clear that dying -- and how you cope with and prepare for it -- is a common factor for all people. Wealth, resources and opportunity get leveled out in those final moments of your life. I heard it echoed many times -- compassion and love is what all of us want in our final hours."
For Living Room, an expanse of the hospice and funeral home services to a second site located near Eldoret town was approved by the Kenyan and U.S. boards. The site is approximately a 35 mile/90 minute drive from Living Room's existing campus and is situated in a strategic location in its nearness to a newly opened cancer center, which provides care to nearly 700 cancer patients/month in the out-patient clinic. Living Room will be the primary referral site enabling many adults and children to receive quality palliative care services. The expansion demonstrates, and adds further credibility to the importance of palliative care to the larger Kenyan health care system.
A second surprise is how the new site was acquired. The day after the decision to expand into Eldoret, Juli received a call from a lady who wanted to donate furniture to Living Room. Her name was Kate, and she explained that her 95 year old mother-in-law had just passed away and had been living on an eight acre farm a few miles from Eldoret town. Kate had come to Kenya for the funeral and to get the estate in order and would shortly be returning to England. Within two weeks of meeting Kate, Living Room was able to purchase the land for half of the valued price. Juli is still astonished by the experience, "the serenity and beauty that fills the place is impossible to describe with words and feels like a gift I did not even know to ask for."
Since 2009 Living Room's Kimbilio Hospice and Funeral Home has provided services to over 1,200 patients and families. The Eldoret site expansion will significantly increase that number and the impact of the documentary as a teaching tool is impossible to measure but undeniable. A lot of hard work, unwavering faith and a bit of good fortune can go a long way.