Strangers and friends alike often ask me how I possibly could have decided to be a gynecologist. "Why would you do that all day?" I prefer instead to answer the question, "Why did you choose to become a comprehensive reproductive health care provider?" -- a slight reframing for which I have a long and beautiful answer. I assume when they ask about 'that' they mean the female anatomy, which must not be named. To that, I say women are so much more than their anatomy and I provide care to more than just one body part.
So here's the long and beautiful answer. It is my privilege to provide comprehensive reproductive health care. What I learn from my patients every day is that every woman's story is different. A woman comes to my office with a lifetime of personal experience. It is not my place to tell her what is right for her. It is my place to empower her to make a decision that's in line with her priorities.
Family planning is one of the top 10 public health achievements of the 20th century and, for millions of women and families, modern birth control makes that planning possible. Birth control can allow a woman to finish an advanced degree, delay childbearing until a life-threatening medical condition is under control, or more easily leave an abusive relationship. Oh, and some methods can improve periods, acne, mood swings and pelvic pain.
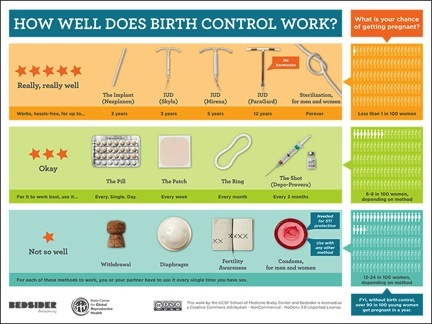
Despite the benefits, there's a lot of misinformation and mythology out there about birth control, so it's important to me to communicate the facts to my patients -- about effectiveness, risks, side effects and benefits -- so they can make an informed decision about the best method for them based on their unique circumstances and values.
Many of my patients have heard a combination of horror stories and downright misinformation -- from TV, great aunts, friends of friends, or the Internet -- and are understandably apprehensive about certain birth control methods. One of the methods with the most mythology is the IUD, which is unfortunate since the IUD is one of the most effective methods available. Modern IUDs are safe and available both with and without hormones.
Speaking of hormones ... So many women come to me believing they aren't candidates for hormonal methods, not realizing that not all hormonal methods are the same. For example, the most common types of birth control pills contain two kinds of hormones -- estrogen and progestin -- while methods like the implant or the IUD only contain progestin. Women who don't do well with estrogen may still feel great using a progestin-only method.
Effectiveness is often at the top of a woman's list of priorities when choosing a method, but many women don't know which methods are most effective. Commonly used methods like the pill and condoms are advertised to be highly effective, but the fine print is that they're only highly effective for people who use them perfectly in research studies. In the real world, almost one in ten women using the pill will get pregnant within a year; almost two in ten will get pregnant using only condoms.
Sometimes my patients feel that they shouldn't be on birth control if they're not in a serious relationship. I fear that this is a response to the stigma that continues to surround birth control even though 99 percent of women have used it at some point in their lives. It breaks my heart to think my patients have internalized negative messages regarding sexuality and self-worth and as a result are embarrassed or ashamed to ask for contraception unless they're in a certain kind of relationship. The reality is that sometimes the most crucial time for effective contraception is early in a relationship!
I've heard so many stories about women's struggles to obtain and continue to use contraception. Some are dramatic, such as my patients with serious cardiac disease or solid organ transplantation who were able to prevent pregnancy while maintaining intimacy during a difficult time in their lives. But even the most 'routine' of visits can open my eyes. I've had patients struggling to make ends meet who are already mothers. They'd like to have more children someday but are currently having trouble providing for the ones they have. By choosing to space childbearing, these moms are making what they feel is the best decision for their entire family, not just for themselves.
As someone with a public health background, I could have written about the 'big picture' benefits of contraception with lots of statistics. When I started down the path of comprehensive reproductive health care, it was these statistics that inspired me. But at the end of the day, it's not statistics that stick with me -- it's patients and their stories.
This post is part of a series produced by The Huffington Post in conjunction with National Women's Health Week, May 11-17. Read all posts in the series here. To learn more, please visit WomensHealth.gov.